On March 24, the world marked the annual Tuberculosis Day. Whereas in Western countries this illness has been controlled since the middle of the 20th century, in Russia, tuberculosis remains an acute problem to this day. IMR Advisor Boris Bruk analyzes the situation and ponders the effectiveness of anti-tuberculosis measures taken by Russian authorities.

Photo by Misha Friedman
On March 24, 1882, at the meeting of the Physiological Society in Berlin, the German bacteriologist Dr. Robert Koch shared his research findings about the discovery of the bacillus that causes tuberculosis (TB). Unfortunately, over 130 years later, the problem of TB still remains unresolved in a number of countries, including Russia.
In the last decades of the nineteenth century, the situation regarding TB was critical: in some cities, the spread of infection reached 100 percent, and in Europe alone, TB caused the death of one in seven people. The Russian annual mortality rate from TB was estimated at 400 deaths per 100,000 persons. The situation was especially severe in prisons, where “the spread of ‘phthisis’ was substantial and isolation of infected persons was often impossible.” For example, in a Yaroslavl prison, the rate of TB infection reached 66 percent.1
With the invention of antibiotics in the 1940s, countries in the West were able to bring the TB situation under control. In the Soviet Union, where the fight against TB became one of “the key objectives of the state healthcare system,” the government announced its victory over TB in the 1970s. This “victory” was achieved through the creation of a centralized system that required mandatory screenings for TB and the immediate isolation of persons infected with TB in sanatoria. Experts suggest that after the disintegration of the Soviet Union, the TB prevention system was deconstructed and that, as a result of the attendant social and economic challenges, declining funding, and “the destruction of [the] monolithic system of control,” the TB situation in Russia was aggravated.2, 3 Among other possible reasons for the resurgence in TB incidence were the increased number of socially vulnerable groups, increased migration from Russia’s “near abroad,” reduced funding for TB departments, a high level of TB infection in prisons, and a higher rate of refusal of vaccination and/or TB screening.
Experts suggest that after the disintegration of the Soviet Union, the TB situation in Russia was aggravated.
During the period from 1991 to 1997, TB rates doubled from 38 to 74 cases per 100,000 persons, while the number of deaths increased on average by 11 percent.4 In addition, an insufficient supply of medications and, consequently, the impossibility of providing the full course of treatment to all affected individuals resulted in cases of multidrug-resistant TB (MDR-TB).
In these conditions, in the 1990s, foreign aid was believed to offer the most timely and effective response. Since 1994, the British NGO MERLIN has worked in close collaboration with the Regional Health Administration and regional tuberculosis services in the Tomsk Oblast. Implementation of the Directly Observed Treatment, Short-course (DOTS) strategy recommended by the WHO led to a 200 percent reduction in the occupancy of hospital beds, a decrease in the amount of time spent in the hospital, and a lower number of cases of TB infection and deaths.5
Additionally, in the second half of the 1990s, with financial support from George Soros, the New York–based Public Health Research Institute (PHRI) started work in Russia. According to Alexander Goldfarb, former project director of the PHRI/Soros Russian TB Program, various Russian “regions were interested in learning about the international experience; they were interested in getting results.” Goldfarb believes that in its initial stages, the program, which “aimed at introducing internationally accepted anti-TB strategies,” was quite successful. Supported by regional authorities, PHRI actively worked with regional health departments in Tomsk, Kemerovo, and Ivanovo. A “constructive cooperation” approach was developed with the Main Directorate for the Execution of Punishments (GUIN). As Goldfarb recollects, however, with the introduction of the initiative to strengthen the “vertical of power," “everything came under the thumb of the Russian Ministry of Health.” In Goldfarb’s words, “The Ministry of Health is an extremely corrupt organization controlled by the pharmaceutical industry, both Russian and foreign. They started putting spokes in our wheels and we had to leave the country.”
The programs of such major international players as the Global Fund to Fight AIDS, Tuberculosis and Malaria and USAID, which started their work in the late 1990s, were implemented for a longer time in Russia. However, in 2011, the Russian Ministry of Health and Social Development decided to decline $127 million in financial assistance from Global Fund sources. This decision resulted in the change of Russia’s status from “recipient” to “donor,” a label that makes the country responsible for contributing $20 million annually during the period from 2011 to 2013. In 2012, USAID, which had participated in the fight against TB in Russia and supported over 200 Russian HIV/AIDS organizations, had to end its programs in the country.
Photo by Misha Friedman
According to Russian NGOs, the “refusal of foreign aid might lead to an outbreak of TB in Russia,” and, according to some reports, in early 2012, the situation did indeed worsen. For example, a number of regional clinics and prisons faced a critical shortage of anti-TB drugs. This perspective is not shared by everyone, though. In the words of a representative from the Russian Ministry of Health, the participation of international organizations, including the Global Fund, did not help to solve the TB problem, but, on the contrary, resulted in lower indicators of death from TB in some Russian regions.
The question about the real reasons for and the timing of the government’s refusal to accept foreign aid remains a topic for discussion. Many analysts and experts point to the political component of this decision. One commentator has stated that “Russia’s limitations on international cooperation are impossible to be considered separately from public ‘patriotic’ campaigns in the country”. Within this context, some conclusions have emphasized the “increased political commitment of the [Russian] federal executive bodies” to solving the TB problem. According to some observers, this political commitment is primarily expressed through the decision to “flood the problem” with money.
At last year’s press conference on the occasion of World TB Day, it was announced that within five years, public expenditures for TB diagnostics and treatment would be increased by almost four times. In 2012, twelve Russian regions received over 6 billion rubles from the federal government for the fight against TB. In 2013, these regions will be granted 1 billion rubles. In this context, according to official estimates, the epidemic TB situation in Russia is being stabilized, with decreasing death rates from TB (a 14.5 percent drop) and a decreasing number of new TB cases (a 9.6 percent drop) in the period from 2008 to 2010.
It is expected that this positive trend will continue. For example, the state-run Program on the Development of Healthcare in the Russian Federation until 2020 (approved in late December 2012) sets such goals as the reduction of the annual number of TB-related deaths to 11.2 cases per 100,000 and the reduction of TB cases to 35. Between 2011 and 2015, Stage 1 of the state program is intended to reduce the annual number of deaths from TB from 14.2 to 12.8 and the annual number of new cases of TB from 73 to 56.
Despite financial investments, announcements about stabilization, and the ambitious plans of the Russian government, the current situation regarding TB does not allow for much optimism. Although in terms of quantity and percentages, there has clearly been no return to Dr. Robert Koch’s times, one should realize that at present, the task of TB prevention and treatment has become much more complex. Given that Russia is currently ranked thirteenth in TB burden among 22 high-burden countries, the consequences of the disease might become catastrophic.
The most recent WHO report suggests that 60 percent of MDR-TB cases are concentrated in four countries: India, China, Russia, and South Africa.
The WHO reports that the number of registered cases of MDR-TB in the world has been constantly increasing and that TB treatment has become a challenging task. The situation is especially troubling in prisons, where, according to the WHO, the spread of TB is almost 100 times higher than among the general population and the share of MDR-TB is estimated to be as high as 24 percent.
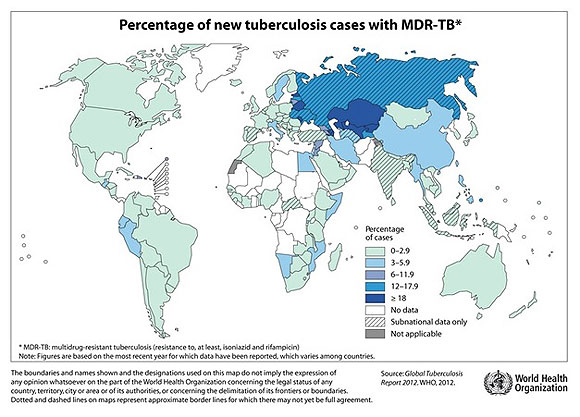
The most recent WHO report on the subject suggests that 60 percent of MDR-TB cases are concentrated in four countries: India, China, Russia, and South Africa. The largest number of patients with MDR-TB reside in Eastern Europe and Central Asia.
The WHO estimates that out of the 630,000 cases of MDR-TB registered in 2011, approximately 9 percent are cases of extensively drug-resistant TB (XDR-TB), the form of TB caused by a strain of bacteria resistant to second-line drugs. A recent study that involved 1,278 TB patients from Estonia, Latvia, Peru, the Philippines, Russia, South Africa, South Korea, and Thailand showed that almost 44 percent of participants demonstrated resistance to at least one second-line drug. Scholars believe that individuals in many post-Soviet countries are infected with TB strains resistant to some antibiotics. The treatment of a drug-resistant strain of TB may take several years, and the cost of treatment can be 200 times more expensive than that required to treat a regular type of TB. The WHO expresses concern for the fact that countries relying on national contributions to treat and control TB—of which Russia is one—face an obvious threat of insufficient funding.
In addition to the problem of drug-resistant types of TB, there is another very serious problem: co-infection HIV/TB. WHO data demonstrate that TB causes one-fourth of all deaths among HIV-infected individuals. Until the mid-1990s, HIV was not considered a problem in Russia. In 1999, however, around 18,000 cases of HIV were registered6. The virus spread quickly, and by the early 2000s, 515 cases of co-infection HIV/TB had been registered7. In 2011, the number of individuals affected by such co-infection was estimated to be almost 12,000. According to official data, during the period from 2004 to 2011, the number of co-infection cases increased by 741 percent.
In this context, Russian organizations of civil society and specialists with first-hand knowledge about TB challenges have argued that the existing system is incapable of solving the problems related to the spread of the infection and of improving the conditions for TB treatment. Against a background of unimpassioned and sometimes opiating official discourse, voices have been raised to emphasize the importance of making every effort to stop TB and defending the rights of TB patients. According to representatives of the Andrey Rylkov Foundation for Health and Social Justice, the system of combating TB must be reformed.
The interview with Anya Sarang, president of the Andrey Rylkov Foundation, is published in the IMR website.
1 Averbukh, L.G. Tuberculosis: Stages of Struggle, Gains and Losses. Odessa, Optimum, 2005.
2 Shilova, M. V., & C. Dye. 2001. The resurgence of tuberculosis in Russia. Philosophical Transactions of the Royal Society of London, Series B, Biological Sciences 356 (1411): 1069–75.
3 Banatvala, N., & G. G. Peremitin. 1999. Tuberculosis, Russia, and the Holy Grail. Lancet 353 (9157): 999–1000.
4 Ibid.
5 Wares, D. F., & C. I. Clowes. 1997. Tuberculosis in Russia. Lancet 350:957.
6 Perelman, M. I. 2000. Tuberculosis in Russia. International Journal of Tuberculosis and Lung Disease. 4:1097–1103.
7 Ibid.